This article draws insights from the research “Data sharing for responsible artificial intelligence in dentistry: a narrative review of legal frameworks and privacy-preserving techniques”, written by Brinz et al. (2025). It aims to help dental lab owners and professionals understand the workflow and principles behind responsible dental data management in the era of digital dentistry.
Table of contents [Show]
Introduction
In today’s digital era, dental data is becoming one of the most valuable assets for modern laboratories. It fuels everything from precision milling and AI-powered diagnostics to smarter workflow automation. Yet despite its potential, data dentistry still lags behind medicine in how effectively it shares and utilizes data across institutions.
Most dental systems remain non-interoperable, meaning they can’t easily exchange information. As a result, labs often work in isolation, limiting access to insights that could enhance production quality and efficiency. Evidence shows how rare open dental data truly is: only 1.5% of 7,509 published dental studies have made their data publicly available. Even in Randomized Controlled Trials (RCTs), which are studies designed to test treatment effectiveness, only 15.8% shared data. This highlights a clear challenge: while the industry recognizes the importance of sharing, few have built the secure frameworks to do it responsibly. Furthermore, low compliance with the FAIR principles: Findable, Accessible, Interoperable, and Reusable limits the potential of dental data. This lack of transparency and connectivity not only slows innovation but also makes it difficult for labs to adopt AI-driven tools that depend on large, high-quality datasets.
For dental labs, this is more than a research issue, but it’s a business opportunity. When managed responsibly, dental data sharing enables smoother collaboration between clinicians, milling centers, and partners. It enhances accuracy, reduces remake rates, and accelerates turnaround times while ensuring compliance with privacy regulations the Health Insurance Portability and Accountability Act (HIPAA) in the United States (US), or the General Data Protection Regulation (GDPR) in the EU.
At XDENT LAB, we see responsible dental data management not only as a compliance requirement but as a foundation for innovation, trust, and growth. By adopting transparent workflows, advanced privacy techniques, and secure collaboration systems, labs can transform how they operate, scale, and serve their partners. As we move toward a future of fully digital dentistry, understanding how to share dental data safely and effectively will define which labs lead the next generation of global collaboration.
To learn more about how XDENT LAB safeguard your information, please visit our Privacy Policy page.
Why Dental Data Sharing Matters for Business Growth
In today’s competitive dental industry, success depends on how effectively labs can connect, collaborate, and deliver. Dental data sharing lies at the heart of this transformation. When managed securely and efficiently, it enables faster communication, smarter automation, and stronger relationships between clinics, technicians, and design teams.
Responsible dental data practices bring measurable business benefits:
Faster collaboration: Secure cloud platforms allow real-time communication and case sharing across locations and time zones.
Reduced errors: Standardized digital workflows minimize miscommunication and production inconsistencies.
Greater client trust: Clinics prefer labs that handle patient information with care — it reflects professionalism and reliability.
Future-readiness: Structured data systems form the foundation for AI-driven design, predictive manufacturing, and scalable operations.
Ultimately, dental data sharing is more than a technical process, it’s a growth strategy. Labs that invest in secure, transparent, and interoperable data systems position themselves as trusted, future-ready partners in the global dental ecosystem.
The Workflow of Responsible Dental Data Sharing
Dental data today come in many forms, e.g. radiographs, CT and cone beam CT scans to intraoral photographs, 3D scans, tabular records, and electronic health records. However, in reality, most dental data are fragmented across disconnected systems that don’t communicate well with one another. Many files are also incomplete or inconsistent, making it difficult to combine or reuse them efficiently. This fragmentation slows down data sharing across institutions. That’s why establishing a clear, standardized data-sharing process is so important, not only to improve interoperability but also to ensure that every file shared between institutions is accurate, compliant, and secure.
The following workflow illustrates a workflow of data sharing (figure 1).
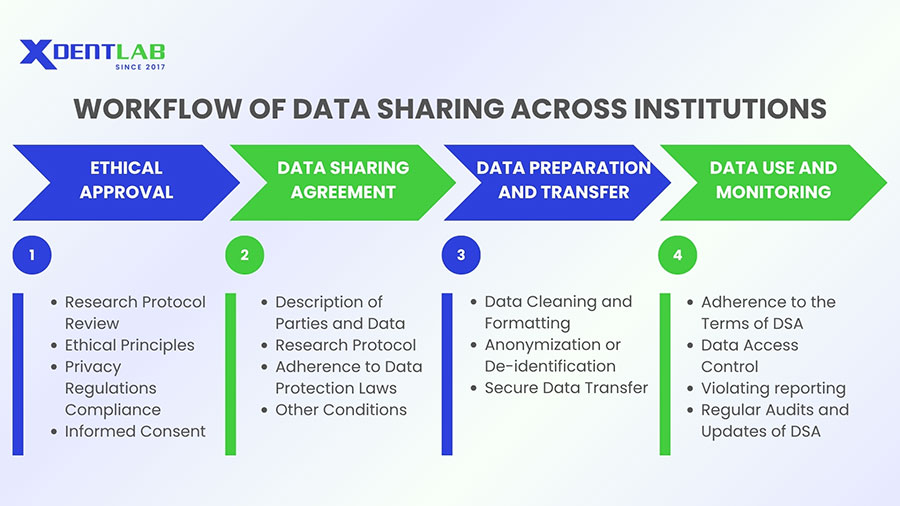
Ethical Approval
Before any dental data is collected, shared, or analyzed, ethical approval forms the foundation of responsible data management. This process ensures that all data handling respects patient privacy, complies with international standards, and upholds professional integrity.
A responsible workflow should always include:
Research protocol review to ensure data is used ethically and appropriately.
Adherence to ethical principles that protect patient rights and transparency.
Compliance with privacy regulations such as GDPR or HIPAA.
Informed consent patients understand, agree to, and can withdraw from data use at any time.
By following these principles, dental labs not only protect sensitive information but also strengthen trust and credibility in every partnership and collaboration.
Data Sharing Agreement (DSA)
Once ethical approval and consent are secured, the next step is to establish a Data Sharing Agreement (DSA). This is a formal document that defines how, why, and with whom dental data can be shared. A clear DSA protects both the data provider (such as a clinic or partner lab) and the data recipient (like a milling center or AI research partner). It outlines responsibilities, usage rights, and data protection measures that ensure every party follows the same standards. The typical content of DSAs is presented in Table 1.
| Parties involved | Identification of institutions providing and receiving the data, including the contact information of responsible employees. |
| Data to be shared | Specific description of the data and associated metadata, their format, expected dataset size. |
| Research protocol | Background information, objectives, description of methodology, risk assessment, approximate timeline of the project. May be included as an annex due to its complexity. |
| Conditions of data sharing | Rights and obligations of each party, including remuneration (if any), intellectual property rights related to the data (ownership, third-party use) and results (publication, licensing). |
| Adherence to data protection laws | Statement of compliance with applicable regulations (e.g. GDPR, HIPAA), including measures to ensure data protection, warranty and liability in case of any security incidents, terms of DSA termination. |
| Annexes | Additional information regarding the project, e.g. detailed research protocol, or amendments to the existing agreement. |
Table 1. Outline of a data-sharing agreement.
Data Preparation and Transfer
Before any dental data is shared, it must be carefully prepared to ensure accuracy, privacy, and compliance. This preparation includes organizing, cleaning and formatting both data (such as intraoral scans, radiographs, or case records) and metadata (like file source, collection date, or case type) so that they can be securely transferred and easily understood by the recipient.
A key part of this process is data de-identification which removes personal identifiers so patients cannot be traced back in case of a data breach. This step is essential when explicit patient consent for data sharing is unavailable, as it helps labs meet global data protection standards such as GDPR and HIPAA. Beyond de-identification, privacy can be strengthened using advanced techniques such as anonymization, pseudonymization, and encryption, which will be discussed later in this article.
The actual sharing of data can be done through secure, encrypted storage devices, data transfer protocols such as SFTP (SSH File Transfer Protocol) or VPN‑protected tunnels, or secure cloud solutions built on zero‑trust architectures, depending on the nature and volume of the data. Both the sending and receiving parties share responsibility for preventing unauthorized access during the transfer. Following frameworks like ISO/IEC 27001:2022 which is the global standard for information security management ensures that your lab operates with internationally recognized safeguards for data handling.
By adopting secure preparation and transfer practices, labs not only protect patient information but also strengthen reliability and trust across digital partnerships, turning responsible data handling into a core business advantage.
Data Use and Monitoring
Once dental data are received, the recipient can use them in accordance with the terms outlined in the Data Sharing Agreement (DSA). Every use must align with the agreed purpose, uphold patient confidentiality, and comply with all ethical and legal standards.
At this stage, maintaining data integrity and security becomes critical. The receiving lab or partner must:
Implement the same protection measures defined in the DSA.
Restrict access strictly to authorized personnel.
Preserve confidentiality across every system and workflow.
If any incident of unauthorized access, privacy breach, or data misuse occurs, the recipient must notify the data provider immediately to minimize potential damage and initiate corrective action.
To ensure long-term trust and compliance, both the provider and receiver should perform regular audits. These audits confirm that:
The shared dental data are used only as permitted.
Security controls remain effective and up to date.
The DSA reflects current laws and technological developments.
This continuous monitoring process is not just about risk prevention, it demonstrates accountability and professionalism. For modern dental labs, such governance turns data ethics into a competitive advantage, strengthening reputation, compliance, and client confidence in every collaboration.
Techniques for Enhancing Dental Data Privacy and Security
Across all modern legal frameworks, one fundamental rule remains consistent: dental data must be de-identified to protect patient privacy. However, in dentistry, achieving full de-identification is uniquely challenging. Because biometric identifiers such as intraoral scans, full-face photographs, and CT or cone beam scans can reveal distinct physical features, this makes dental data inherently more traceable. Even when obvious identifiers (like names or IDs) are removed, indirect clues in images or 3D models can still enable re-identification. That’s why dental labs, software providers, and research partners must apply advanced privacy-preserving techniques.
In the following section, we’ll introduce several methods that enhance the security, efficiency, and reliability of dental data sharing. These techniques bridge the gap between legal obligations and real-world implementation, allowing labs to collaborate, and scale responsibly while keeping patient information safe. The different techniques are summarized in Figure 2.
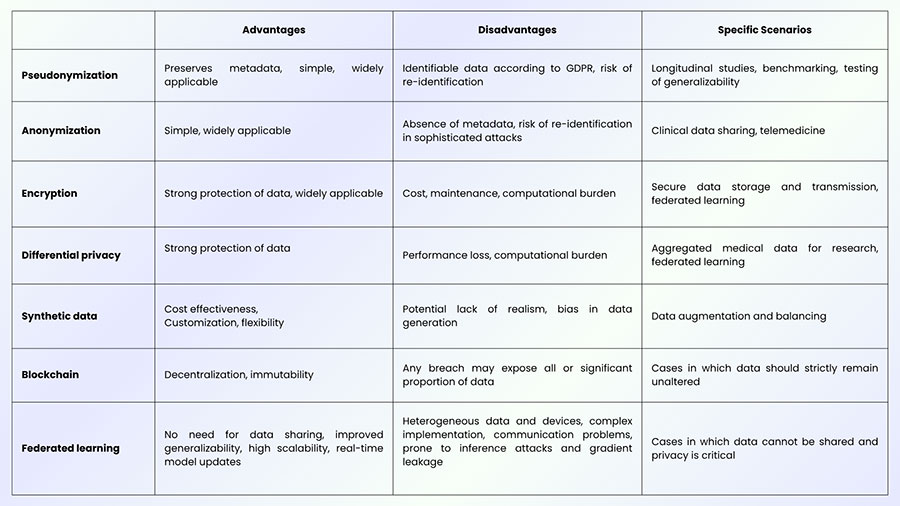
Pseudonymization
Pseudonymization is one of the most practical first steps toward protecting dental data privacy. In this process, identifiable information such as names, patient IDs, or case references is replaced with random alphanumerical identifiers. This makes it impossible to identify individuals directly from the data alone. However, pseudonymization is a reversible process, i.e. individuals can be re-identified if additional information, such as a key, is available. That’s why best practices require this key to be stored separately, with strict access control and limited authorization, ensuring that only approved personnel can access it when necessary.
Nevertheless, under the General Data Protection Regulation (GDPR), pseudonymized data are still considered identifiable, meaning they must be handled in compliance with strict data protection rules.
Anonymization
Anonymization is the process of removing all identifiable information from dental data to ensure that individual patients cannot be traced. It’s one of the most important steps in responsible data handling, especially when sharing data for research, AI training, or multi-lab collaboration.
However, anonymization is not as simple as deleting names or birthdates. Studies show that even after removing direct identifiers (like names, addresses, or patient IDs), indirect clues such as age, treatment date, or scan type can still make re-identification possible when cross-referenced with other datasets.
To reduce these risks while maintaining useful data for AI and research, several anonymization techniques are commonly applied:
Data Swapping: Exchanges certain values between patient records (for example, switching the ages or regions of two cases) to protect identity while preserving statistical relationships.
Generalization: Converts specific data into broader categories, such as replacing “age 46” with “age 40–50” to make individual identification less likely.
Suppression: Removes rare or highly sensitive attributes (for example, extremely uncommon procedures) that could single out a person.
In addition to these basic methods, more advanced mathematical models are used to ensure stronger privacy protection:
k-Anonymity: Ensures that each record in a dataset is indistinguishable from at least k−1 other records.
l-Diversity: Adds diversity to sensitive data values so that even within the same group, individuals cannot be inferred.
t-Closeness: Keeps the distribution of sensitive attributes (like age or gender) similar across different subsets of data.
These methods can be applied individually or in combination, depending on the dataset and its intended use. The key challenge is finding the right balance between privacy and data utility. Over-anonymization can make data useless for AI model development or clinical insights, while under-anonymization can put patient privacy at risk. The best approach is one that preserves analytical value while guaranteeing ethical, secure handling of all dental data.
Encryption
Homomorphic Encryption (HE) is an advanced method of protecting dental data that allows computations to be performed without ever revealing the original data. In simpler terms, HE lets computers analyze encrypted information, for example, to measure trends, train AI models, or calculate averages without needing to decrypt it first. The data remains locked and unreadable during the entire process. Once the calculation is complete, the result can be decrypted, and it will be identical to what you would get if the operation had been performed on the unencrypted data.
The most advanced form of HE, called Fully Homomorphic Encryption (FHE), is commonly applied in the medical and bioinformatics fields when using machine learning techniques, as it allows for complex analyses of sensitive information (e.g., medical records, genomic data) without exposing individual details.
Differential privacy
Differential Privacy (DP) is a statistical method that allows researchers and AI systems to learn from dental data without revealing sensitive information about any individual patient. In practice, DP works by adding a small, carefully controlled amount of “noise” (random variation) to the dataset or the results of data analysis. This makes it difficult to trace any data point back to a specific person even if the dataset is later combined with other information sources. For example, when training an AI model on dental imaging data, Gaussian Differential Privacy adds random noise to either the data itself or the model’s parameters during the learning process. This protects patient confidentiality while still allowing the AI to detect meaningful patterns, such as tooth structure, decay, or implant fit.
However, there’s always a trade-off: the more noise added, the stronger the privacy but the lower the model’s accuracy. Striking the right balance between privacy and performance is a key challenge when applying DP in dental AI research and lab-to-lab collaboration.
Synthetic data
Synthetic data generation is an emerging technique designed to protect privacy while still enabling innovation with dental data. Instead of using real patient records, this method creates artificial datasets that imitate the patterns and statistical properties of real-world data. For example, synthetic data can be generated to reflect real clinical cases such as tooth morphology, cavity types, or implant placements without exposing any actual patient information. This approach allows dental labs and researchers to train AI models, test workflows, or validate algorithms safely and ethically.
One major advantage of synthetic data is that it helps expand limited datasets and reduce bias in AI training, especially when real data are scarce or legally restricted from sharing. However, the trade-off is that models trained solely on synthetic data may not perform as accurately as those trained on real-world patient data.
Even so, synthetic data is becoming a valuable bridge between data privacy and AI advancement, allowing the dental industry to explore powerful new applications while maintaining patient confidentiality and regulatory compliance.
Blockchain
Blockchain technology offers a new way to manage and protect dental data by replacing traditional centralized systems with a secure, decentralized network. In a blockchain system, data are divided into small pieces called “blocks”, which are securely linked together in order, forming a “chain”. Instead of storing data in one single location, identical copies are distributed across multiple computers or servers (known as nodes). This structure ensures that no single organization controls all the information, making data tampering and unauthorized access far more difficult.
Because every change must be verified by the network, blockchain provides strong protection against data manipulation and creates a permanent, traceable record of all transactions. For dental labs, this means greater accountability, transparency, and trust when sharing data between clinics, design partners, and AI systems.
However, blockchain isn’t without challenges. Since data stored on the blockchain cannot be easily modified or deleted, it can conflict with privacy laws such as the GDPR, which grants individuals the “right to be forgotten.” In addition, because each node contains a copy of the data, a breach in one node could still compromise confidentiality.
Despite these limitations, blockchain remains a promising tool for secure data exchange and traceability in dentistry, particularly when combined with other privacy-enhancing technologies like pseudonymization and encryption. As the industry continues to digitalize, blockchain could play a key role in building trustworthy, tamper-resistant dental data ecosystems.
Federated learning
While the techniques enhancing privacy and security provide robust methods for protecting data during storage and transmission, they may not fully address the challenges of maintaining data security in distributed systems where information is processed across multiple entities. To address this gap, emerging paradigms such as federated learning (FL) offer a promising solution. FL enables collaborative model training without sharing raw data, thereby preserving privacy while still benefiting from decentralized data sources.
Here’s how it works:
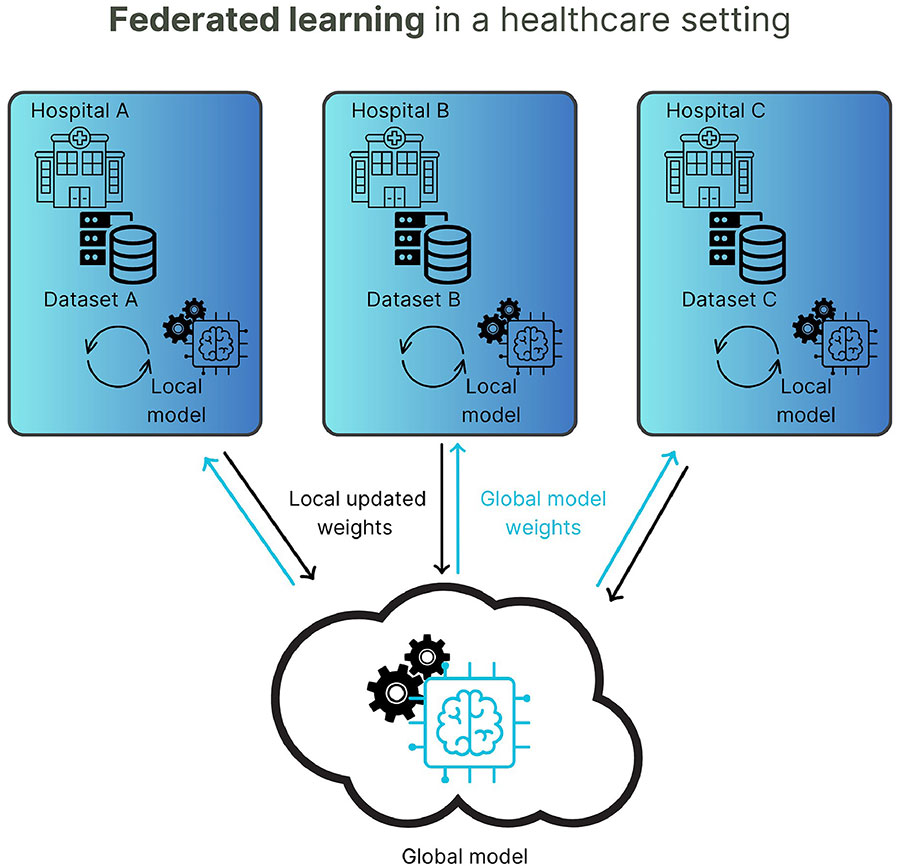
Each participating dental lab or clinic keeps its data securely on-site. The AI model is sent to each location, learns from the local data, and only sends the updated model parameters (not the actual data) back to a central server. These updates are then combined to improve the overall AI system.
This process allows multiple labs, clinics, or research institutions to collaborate and build powerful AI systems without ever sharing identifiable patient information. It’s particularly valuable in dentistry, where datasets such as radiographs, CT scans, or intraoral images are sensitive and vary across institutions.
The benefits of federated learning include:
Enhanced privacy: Sensitive dental data never leaves the local environment.
Better generalization: Models trained on diverse data from multiple labs perform more accurately in real-world scenarios.
Reduced legal complexity: Since raw data are not exchanged, compliance with privacy laws like the GDPR or HIPAA becomes easier.
However, federated learning requires strong coordination, consistent data quality, and secure communication channels to prevent potential cyber threats during parameter exchanges.
For forward-thinking dental labs, federated learning represents a strategic opportunity, enabling AI innovation and collaboration while upholding the highest standards of data security and patient trust.
Conclusion
The evolution of digital dentistry is driven by data and how responsibly we manage, protect, and share that data defines the future of our industry. For modern dental labs, trust and transparency are no longer optional; they are the foundation of every successful collaboration.
At XDENT LAB, we believe that responsible dental data management is the key to building stronger global partnerships. Every case submission begins with our Magic Touch Portal, a dedicated platform that streamlines communication, ensures traceability, and maintains data integrity throughout the production workflow. For larger digital assets, we also support transfers via We Transfer, a globally recognized tool that allows seamless, secure file exchange for clients around the world.
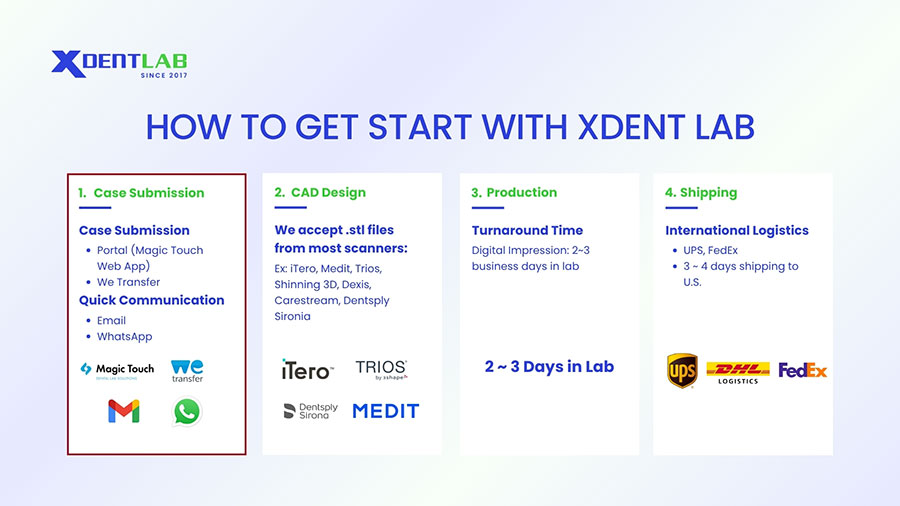
This dual-system approach reflects our commitment to both security and accessibility, combining a professional in-house infrastructure with international best practices. Though based in Vietnam, XDENT LAB operates at a global standard, ensuring that each restoration is not only crafted with precision but also handled with the highest respect for patient data privacy. By embracing digital responsibility and advanced technology, we position ourselves as more than a production lab: we are your trusted digital partner, helping labs work smarter, faster, and more securely.
XDENT LAB is an expert in Lab-to-Lab Full Service from Vietnam, with the signature services of Removable & Implant, meeting U.S. market standards – approved by FDA & ISO. Founded in 2017, XDENT LAB has grown from local root to global reach, scaling with 2 factories and over 100 employees.. Our state-of-the-art technology, certified technicians, and commitment to compliance make us the trusted choice for dental practices looking to ensure quality and consistency in their products.

Our commitments are:
100% FDA-Approved Materials.
Large-Scale Manufacturing, high volume, remake rate < 1%.
2~3 days in lab (*digital file).
Your cost savings 30%.
Uninterrupted Manufacturing 365 days a year.
Contact us today to establish a strategy to reduce operating costs.
--------❃--------
Vietnam Dental Laboratory - XDENT LAB
🏢 Factory 1: 95/6 Tran Van Kieu Street, Binh Phu Ward, Ho Chi Minh City, Vietnam
🏢 Factory 2: Kizuna 3 Industrial Park, Can Giuoc Commune, Tay Ninh Province, Vietnam
☎ Hotline: 0919 796 718 📰 Get detailed pricing
Tags:
Digital DentistryShare this post: