Explore the components of RPD, their biomechanical functions, and design principles for optimal removable partial denture performance.
Table of contents [Show]
Abstract
Removable Partial Denture (RPD) is a fundamental treatment modality in prosthodontics, especially for patients with partial edentulism who still retain natural abutment teeth. The design and fabrication of RPD require close collaboration between clinicians and dental laboratory technicians, grounded in biomechanics, anatomy, and occlusal principles. This article provides a comprehensive and academic overview of the components of RPD, analyzing the biomechanical role of each element, essential design requirements, and the clinical significance of proper framework construction in modern removable prosthodontics.
Introduction
In the rehabilitation of partial tooth loss, RPD occupies a unique position due to its flexibility, conservative nature, and cost-effectiveness. Compared to fixed prostheses or implant-supported restorations, RPD can be applied in a wide range of complex clinical situations, including extensive edentulous spans, severe alveolar ridge resorption, financial limitations, or contraindications to implant therapy.
However, the long-term clinical success of RPD depends largely on framework design and structural integrity. A well-designed RPD ensures:
Optimal distribution of occlusal forces
Preservation of abutment teeth and supporting tissues
Enhanced stability and retention
Improved patient comfort and adaptability
Therefore, a thorough understanding of the components of RPD is essential in both dental education and clinical practice.
Structural Overview of RPD
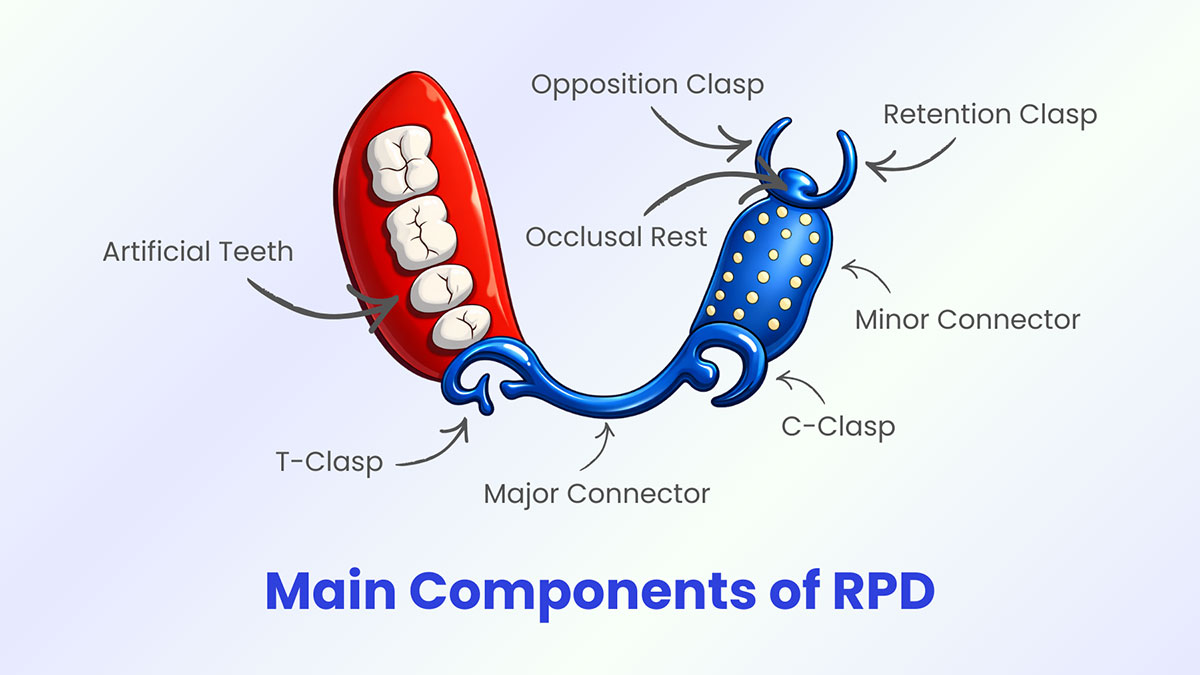
A standard removable partial denture consists of five major component groups:
Major connector
Minor connector
Clasp assembly
Acrylic base
Artificial teeth
Each component plays a critical role in force distribution, structural stability, and biological compatibility.
Major Connector
Definition
The major connector is the primary metal framework element that unites all parts of the RPD into a single rigid structure. In the maxilla, it typically extends across the palate, whereas in the mandible, it traverses the lingual sulcus or floor of the mouth.
Biomechanical Role
The major connector is essential for:
Transmitting occlusal forces from one side of the arch to the other
Distributing masticatory loads evenly across supporting structures
Enhancing overall rigidity and resistance to deformation
Inadequate rigidity of the major connector can result in stress concentration on abutment teeth or soft tissues, leading to bone resorption, periodontal damage, and prosthetic failure.
Design Requirements
High rigidity with minimal bulk
Minimal interference with soft tissues
No obstruction to speech or swallowing
Ease of hygiene maintenance
Minor Connector
Definition
Minor connectors are metal struts that connect the major connector to clasp assemblies, rests, and the acrylic base.
Functions
Transmit occlusal forces from artificial teeth to the framework
Stabilize clasp components and rests
Maintain structural unity of the prosthesis
Design Principles
Short and rigid
Minimal tissue coverage
Avoidance of plaque-retentive areas
Unobstructed path of insertion and removal
Clasp Assembly
The clasp assembly consists of three essential components: the retention clasp, the opposition (reciprocal) clasp, and the occlusal rest.
Retention Clasp
Function
The retention clasp provides resistance against dislodging forces, preventing accidental displacement of the prosthesis during mastication, speech, and swallowing.
Biomechanical Principle
Retention is achieved by engaging the natural tooth undercut, allowing elastic deformation of the clasp during insertion and removal, followed by complete recovery.
Design Criteria
Adequate flexibility
Minimal stress on abutment teeth
Optimal esthetics
Opposition Clasp (Reciprocal Arm)
Function
The opposition clasp counteracts the lateral forces generated by the retention clasp, stabilizing the abutment tooth during prosthesis insertion and removal.
Biological Significance
Without reciprocal stabilization, lateral forces may cause tooth tipping, periodontal ligament trauma, and alveolar bone resorption.
Occlusal Rest
Function
Prevents vertical displacement of the prosthesis
Directs occlusal forces along the long axis of abutment teeth
Protects soft tissues from excessive load
Clinical Importance
Occlusal rests ensure that masticatory forces are primarily transferred to abutment teeth rather than compressible mucosa, thereby preserving residual ridge integrity.
Acrylic Base
Function
The acrylic base supports artificial teeth and simulates gingival tissues, contributing to both functional stability and esthetics.
Biological Requirements
Excellent tissue compatibility
Absence of irritation or allergic reaction
Accurate adaptation to the underlying mucosa
Esthetic Role
The acrylic base restores natural gingival contours and soft tissue emergence profiles, enhancing the overall appearance of the prosthesis.
Artificial Teeth
Function
Artificial teeth restore mastication, phonetics, and facial esthetics.
Technical Requirements
Anatomical morphology appropriate to arch form
Harmonized occlusion
Natural shade and translucency
Biomechanical Principles in RPD Design
An optimal RPD design must comply with fundamental biomechanical principles:
Even distribution of occlusal forces
Maximization of tissue support area
Minimization of unfavorable lever arms
Optimization of the path of insertion
Adherence to these principles significantly enhances prosthesis longevity and preserves oral structures.
Conclusion
A comprehensive understanding and precise application of the components of RPD form the cornerstone of successful removable prosthodontic therapy. Scientifically sound framework design not only ensures clinical effectiveness but also significantly improves patient comfort and quality of life. For clinicians and dental technicians alike, continuous advancement in academic knowledge and design expertise is essential for achieving excellence in removable prosthodontics.
XDENT LAB is an expert in Lab-to-Lab Full Service from Vietnam, with the signature services of Removable & Implant, meeting U.S. market standards – approved by FDA & ISO. Founded in 2017, XDENT LAB has grown from local root to global reach, scaling with 2 factories and over 100 employees.. Our state-of-the-art technology, certified technicians, and commitment to compliance make us the trusted choice for dental practices looking to ensure quality and consistency in their products.

Our commitments are:
100% FDA-Approved Materials.
Large-Scale Manufacturing, high volume, remake rate < 1%.
2~3 days in lab (*digital file).
Your cost savings 30%.
Uninterrupted Manufacturing 365 days a year.
Contact us today to establish a strategy to reduce operating costs.
--------❃--------
Vietnam Dental Laboratory - XDENT LAB
🏢 Factory 1: 95/6 Tran Van Kieu Street, Binh Phu Ward, Ho Chi Minh City, Vietnam
🏢 Factory 2: Kizuna 3 Industrial Park, Can Giuoc Commune, Tay Ninh Province, Vietnam
☎ Hotline: 0919 796 718 📰 Get detailed pricing
Share this post:





