Evidence-based review of resin-based sealants: chemistry, types, retention rates, and clinical protocols for superior pit and fissure caries prevention.
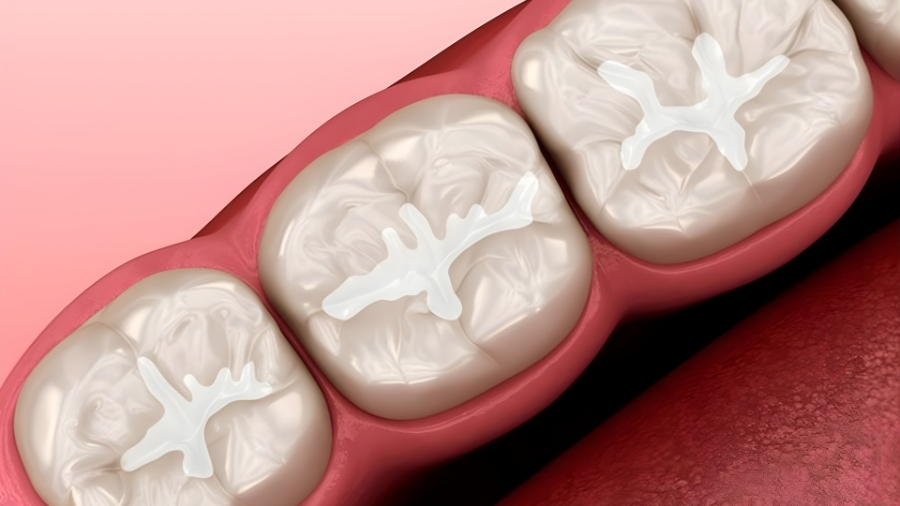
Table of contents [Show]
- Overview
- Historical Development
- Chemical Composition
- Types of Resin-Based Sealants
- Physical & Mechanical Properties
- Clinical Application Technique
- Clinical Performance
- Factors Affecting Success
- Advanced Formulations
- Special Clinical Situations
- Quality Control & Assessment
- Complications & Management
- Safety Considerations
- Cost-Effectiveness Analysis
- Recent Research & Innovations
- Clinical Guidelines & Recommendations
- Future Directions
- Conclusion
- XDENT LAB Perspective (Quality & Consistency)
Overview
Resin-based sealants (RSs) are widely regarded as the gold standard for pit and fissure protection due to superior retention and proven caries prevention. While glass ionomer sealants provide fluoride release and moisture tolerance benefits, RSs consistently deliver longer-lasting occlusal coverage when isolation is adequate. Ongoing innovations—moisture-tolerant chemistries, bioactive fillers, and nano-engineering—continue to refine performance. Comparative studies between flowable composites and moisture-tolerant RSs highlight the field’s shift toward materials that balance retention with clinical practicality in challenging environments.
Historical Development
A concise evolution explains current material capabilities and technique expectations.
Evolution of Resin Sealants
1955: Buonocore introduces acid-etching, enabling micromechanical retention.
1960s: Cyanoacrylate sealants (poor retention; largely abandoned).
1970s: BIS-GMA resin sealants adopted.
1980s: Visible light-cured systems improve handling and set control.
1990s–present: Fluoride-releasing, radiopaque, and moisture-tolerant formulations.
Material Advancement
First generation: Chemically cured resins.
Second generation: UV light-cured resins.
Third generation: Visible light-cured resins with better conversion.
Fourth generation: Fluoride-releasing systems.
Current generation: Bioactive, smart, and hydrophilic/“moisture-tolerant” systems.
Chemical Composition
Core chemistry underpins flow, bonding, polymerization, and wear behavior.
Resin Matrix Components
BIS-GMA (≈40–60%): Primary structural monomer.
TEGDMA (≈20–40%): Diluent to reduce viscosity and improve flow.
UDMA/BIS-EMA: Alternatives to tune viscosity and mechanical strength.
HEMA: Hydrophilic monomer used in some moisture-tolerant systems.
Additives: Inhibitors, stabilizers, and silane coupling agents.
Polymerization System
Photoinitiators: Camphorquinone (≈0.2–1%) as main initiator.
Co-initiators: Tertiary amines to enhance activation.
Accelerators: Optimize polymerization rate and depth.
UV stabilizers: Maintain color stability during service.
Filler Systems
Inorganic fillers (0–50% by weight): Silica/glass for wear resistance.
Radiopaque glass: Improves detectability on radiographs.
Fluoride-containing fillers: Therapeutic release and recharge potential.
Nano-fillers: Increase mechanical strength and polish, modulate viscosity.
Types of Resin-Based Sealants
Material selection should reflect fissure anatomy, isolation feasibility, and target longevity.

Unfilled Resin Sealants
Clear/transparent, low viscosity.
Superior penetration into narrow fissures.
Easier application, but lower wear resistance.
Useful as a “first pass” in very fine fissures or over bonding agents.
Filled Resin Sealants
Opaque/white; higher viscosity with improved wear resistance.
Better mechanical properties and longevity.
Radiopaque options aid follow-up detection.
Preferred when occlusal load and abrasion are concerns.
Fluoride-Releasing Resin Sealants
Sustained fluoride release and recharge.
Comparable handling to conventional resins.
Dual benefit: physical barrier plus chemical protection.
Moisture-Tolerant Formulations
Hydrophilic monomers improve performance in partially erupted teeth.
Better wet bonding, lower technique sensitivity than conventional RSs.
Valuable in pediatric, special needs, and public health settings.
Physical & Mechanical Properties
Performance depends on flow, conversion, and resistance to occlusal stresses.
Viscosity & Flow
Low viscosity (≈0.5–2.0 Pa·s) for deep fissure penetration.
Good wetting (contact angle <30°) improves micromechanical interlock.
Thixotropic behavior desirable for placement control.
Polymerization Characteristics
Depth of cure: ≈2–3 mm, product-dependent.
Polymerization shrinkage: ≈2–5%; minimized by thin film application.
Degree of conversion: ≈50–70% typical for light-cured systems.
Working/setting: Unlimited working time; 20–40 s light cure per site.
Mechanical Properties (typical ranges)
Flexural strength: ≈80–120 MPa.
Compressive strength: ≈200–300 MPa.
Tensile strength: ≈30–50 MPa.
Hardness: ≈15–40 KHN.
Wear resistance improves with fillers and high conversion.
Clinical Application Technique
Standardized protocols maximize retention and minimize failures.

Tooth Preparation Protocol
Prophylaxis with non-fluoridated pumice to remove pellicle/debris.
Rinse thoroughly.
Isolation—rubber dam preferred; high-quality alternatives acceptable.
Drying—oil-free air; maintain desiccation.
Inspect for cavitation or dentinal involvement.
Acid Etching Procedure
Etchant: 35–37% phosphoric acid.
Time: 15–20 s on permanent teeth (shorter for hypoplastic enamel).
Extend etch 2–3 mm beyond fissures.
Rinse for equal duration; dry to frosted appearance.
Sealant Application
Apply via brush/syringe; avoid air bubbles (use explorer to tease out).
Allow 15–20 s for flow into supplemental grooves.
Consider bonding agents in difficult retention cases (per IFU).
Light Curing Protocol
Wavelength: ≈470 nm; intensity ≥400 mW/cm².
Tip distance: <2 mm; cure 20–40 s per segment.
Overlap curing for large occlusal surfaces.
Clinical Performance
Evidence supports robust prevention when technique is controlled.
Retention Rates
1 year: 85–95% complete retention.
3 years: 70–85% complete.
5 years: 50–70% complete; partial retention adds protective value.
10 years: 30–50% still intact in well-maintained cases.
Effectiveness Data
Immediate: full occlusal coverage prevents new lesions on sealed grooves.
2 years: ≈80–90% caries reduction.
5 years: ≈60–70% reduction with maintenance.
Strong cost-effectiveness in high-risk teeth and populations.
Comparative Performance
Resin-based vs GI: RSs show superior long-term retention under ideal isolation.
Compomers: Intermediate performance; more technique sensitive than GI.
Flowable composites: Can approach RS retention in some studies when used as sealants.
Moisture-tolerant RSs: Improved outcomes where isolation is challenging.
Factors Affecting Success
Operator control and patient factors drive longevity.
Moisture Control
Saliva contamination is the leading cause of failure.
Rubber dam or optimized isolation (four-handed dentistry) recommended.
High-volume suction and retraction devices reduce contamination risk.
Technique Variables
Adequate etching and a sustained dry field are non-negotiable.
Appropriate viscosity for fissure anatomy increases penetration.
Sufficient light intensity and exposure ensure conversion.
Operator experience correlates with reduced failures.
Patient Factors
Eruption status and age affect isolation and access.
Fissure complexity and tooth position influence material choice.
Diet and plaque control maintain margins and reduce failure risk.
Adherence to recalls enables timely repair/reapplication.
Advanced Formulations
Next-gen RSs aim for chemical protection and smarter behavior.
Bioactive Resin Sealants
Calcium phosphate or bioactive glass additives for remineralization.
pH-responsive release and antimicrobial agents.
Self-healing microcapsules under investigation.
Nanotechnology Applications
Nano-fillers enhance strength, polish, and flow.
Nano-structured surfaces may improve micromechanical retention.
Antibacterial nanoparticles for biofilm modulation (research phase).
Color-Changing Technology
Placement visibility and curing indicators improve QA.
Wear monitoring aids recall decisions and patient education.
Special Clinical Situations
Tailor protocols to clinical constraints and tooth conditions.
Partially Erupted Teeth
Choose moisture-tolerant RSs or GI as interim with later RS replacement.
Stage sealing as eruption progresses.
Increase monitoring interval (e.g., every 3 months).
Hypoplastic Enamel
Consider reduced etch times and selective bonding.
Use filled RSs for enhanced durability.
Extend coverage beyond defects and monitor closely.
Previously Sealed Teeth
Partial loss: clean, re-etch, and repair.
Complete loss: full reapplication; reassess isolation strategy.
Document prior materials and batch numbers.
Quality Control & Assessment
Embedding QA steps elevates program-level outcomes.
Immediate Evaluation
Confirm continuous coverage and smooth margins.
Explorer check for voids; remove excess and adjust occlusion.
Verify cure parameters (time, intensity) and document.
Follow-Up Protocol
3 months: initial integrity check in high-risk/erupting teeth.
6 months: routine evaluation; annual thereafter.
Risk-based recall scheduling and standardized documentation.
Complications & Management
Early detection and remediation sustain protective benefit.
Common Failures
Complete or partial loss.
Marginal defects and staining.
Bulk fracture (more common in filled RSs).
Discoloration affecting monitoring.
Failure Management
Same-visit repair when feasible.
Full replacement if extensive loss.
Switch to moisture-tolerant RS or GI in persistent contamination.
Reinforce isolation technique and patient education.
Safety Considerations
Risk remains low with modern materials and technique controls.
BPA Concerns
Trace BPA-related species may be detected briefly post-placement.
Levels are well below safety thresholds; BPA-free options available.
Wipe/air-water spray after cure to reduce residuals.
Allergic Reactions
Rare methacrylate sensitivity; document histories.
Provide operator PPE and ventilation for uncured monomer exposure.
Select alternative materials for sensitive individuals.
Cost-Effectiveness Analysis
Sealants reduce restorative burden and downstream costs.
Economic Benefits
Cost per tooth ≈ $30–60; savings ≈ $60–200 per tooth.
Break-even typically within 3–5 years.
Societal benefits include fewer emergencies and productivity gains.
Program Implementation
Risk-based, school-based programs maximize ROI.
Auxiliary-led placement under standardized protocols reduces costs.
Portable setups extend reach to underserved populations.
Recent Research & Innovations
Evidence and engineering are converging on smarter, more durable sealants.
Smart Materials
pH-triggered therapeutic release and biofilm-responsive antimicrobials.
Self-indicating wear features.
Toward personalized, risk-stratified formulations.
Application Technologies
Air abrasion and laser etching as adjuncts in select cases.
CAD/CAM-guided delivery and robotics (exploratory).
Digital monitoring and AI-supported assessments for QA.
Clinical Guidelines & Recommendations
Consensus supports proactive, risk-based deployment.

Evidence-Based Protocols
ADA/AAPD endorse sealing sound or non-cavitated occlusal surfaces.
Technique standards emphasize isolation and adequate cure.
Use measurable outcomes (retention, caries incidence) for QA.
Decision-Making Criteria
Caries risk status and fissure morphology guide placement.
Immediate post-eruption timing improves outcomes.
Consider alternative materials when isolation is compromised.
Future Directions
The next wave aims for longer retention and integrated therapeutics.
Material Development
Enhanced adhesion systems resilient to moisture.
Targets for >10-year retention with minimal maintenance.
Multimodal therapeutic delivery (fluoride, calcium/phosphate, antimicrobials).
Clinical Applications
Expanded adult indications for deep fissures at risk.
Therapeutic sealing over early non-cavitated lesions.
Simplified protocols for global health and outreach programs.
Conclusion
Resin-based sealants remain the gold standard for occlusal caries prevention when isolation and technique are controlled, offering excellent retention and cost-effective protection. Modern variants—fluoride-releasing, radiopaque, and moisture-tolerant—extend usability across clinical scenarios, including partially erupted teeth and public health settings. With continuous innovations in bioactive chemistry and nanotechnology, RSs are poised to deliver longer-lasting, smarter protection. Consistent protocols, rigorous QA, and risk-based follow-up ensure predictable outcomes and scalable quality across multi-site practices.
XDENT LAB Perspective (Quality & Consistency)
For practices partnering with XDENT LAB’s FDA/ISO-aligned lab-to-lab services, standardizing sealant workflows—documented isolation methods, cure parameters, material/batch tracking, and risk-based recalls—drives consistent outcomes across locations. Embedding these controls into preventive programs supports predictable, compliant care and reduces variability, matching the needs of dental groups focused on quality and long-term patient protection.
XDENT LAB is an expert in Lab-to-Lab Full Service from Vietnam, with the signature services of Removable & Implant, meeting U.S. market standards – approved by FDA & ISO. Founded in 2017, XDENT LAB has grown from local root to global reach, scaling with 2 factories and over 100 employees.. Our state-of-the-art technology, certified technicians, and commitment to compliance make us the trusted choice for dental practices looking to ensure quality and consistency in their products.

Our commitments are:
100% FDA-Approved Materials.
Large-Scale Manufacturing, high volume, remake rate < 1%.
2~3 days in lab (*digital file).
Your cost savings 30%.
Uninterrupted Manufacturing 365 days a year.
Contact us today to establish a strategy to reduce operating costs.
--------❃--------
Vietnam Dental Laboratory - XDENT LAB
🏢 Factory 1: 95/6 Tran Van Kieu Street, Binh Phu Ward, Ho Chi Minh City, Vietnam
🏢 Factory 2: Kizuna 3 Industrial Park, Can Giuoc Commune, Tay Ninh Province, Vietnam
☎ Hotline: 0919 796 718 📰 Get detailed pricing
Share this post:





