Dental AM deep dive: SLS vs MJF for orthodontics, prosthodontics, implants, and guides. Learn design rules, tolerances, and QA to scale reliable production.

Table of contents [Show]
- Context and Scope
- Overview of 3D Printing Technologies in Dentistry
- Selective Laser Sintering (SLS) in Dental Applications
- Multi Jet Fusion (MJF) in Dental Applications
- Key Dental Applications
- Material Requirements for Dental Applications
- Biocompatibility and Safety Considerations
- Advantages of SLS/MJF for Dental Manufacturing
- SLS vs MJF: Comparative Insights
- Process Control, QA, and Compliance
- Decision Framework for Dental Use Cases
- XDENT LAB Perspective
Context and Scope
Selective Laser Sintering (SLS) and Multi Jet Fusion (MJF) are powder‑bed fusion technologies increasingly used in dentistry for orthodontics, prosthodontics, implantology, maxillofacial surgery, and tissue‑related applications. Both build parts from thermoplastic powders without support structures, enabling accurate, repeatable production. For dental practices and labs, the core decision hinges on process physics, material options, dimensional accuracy, throughput, and compliance. XDENT LAB focuses on FDA/ISO‑aligned workflows that turn additive manufacturing into reliable, audit‑ready outcomes.
Overview of 3D Printing Technologies in Dentistry
Dental additive manufacturing leverages several platforms, including stereolithography (SLA), selective laser sintering/melting (SLS/SLM), and agent‑assisted fusion (MJF). SLA dominates for highly smooth, photopolymer parts, while SLS/SLM and MJF excel at durable, end‑use components in nylon (PA12/PA11), TPU, and metal alloys, serving appliances, models, jigs, guides, and select frameworks.
Selective Laser Sintering (SLS) in Dental Applications

Historical Development
SLS was conceived by Dr. Carl Deckard and Dr. Joe Beaman at the University of Texas in the 1980s, establishing powder‑based additive manufacturing that later enabled dental devices and research‑grade parameter control.
Materials and Applications
Polymers: PA12/PA11 for appliances, jigs, models; TPU for flexible components.
Metals: Co‑Cr and other alloys via laser sintering/melting for crowns, bridges, and substructures; glass‑ceramic powders explored for restorations.
Use cases: custom trays, splints, occlusal guards, denture bases, surgical guides, and functional housings.
Why Polymer SLS Leads in Dental Appliance Manufacturing
No support structures: complex geometries and efficient depowdering.
Mechanical robustness: near‑isotropic strength, abrasion resistance, and stable dimensions.
Process openness: tunable parameters for fit, density, and surface quality.
Biocompatibility
Several SLS‑processed polymers (e.g., PCL, PLLA, PA grades with medical‑use formulations) have been evaluated for biocompatibility and demonstrate cell adhesion and proliferation potential. Material selection must align with ISO 10993 evaluations and device‑specific regulatory requirements.
Multi Jet Fusion (MJF) in Dental Applications
Technology Overview
MJF spreads powder layers and deposits fusing and detailing agents selectively, then applies infrared energy to solidify treated regions. This agent‑assisted approach improves detail resolution and reduces cycle time, making it attractive for scaled dental production.
Revolutionary Applications in Clear Aligners
MJF is widely used to print aligner molds and orthodontic models, enabling rapid, accurate, and repeatable throughput for clear aligner workflows. The speed and edge sharpness drive better thermoforming outcomes and predictable finishing.
Industrial‑Scale Production
MJF supports concept models, rapid prototypes, and direct digital manufacturing of dental appliances. Nylon parts exhibit strong mechanical properties suitable for functional use, with stable batch‑to‑batch performance.
Design Considerations
Orientation: optimize for dimensional stability and accessible depowdering.
Feature limits: respect minimum wall thickness, hole diameters, and text height for legibility.
Tolerances: apply GD&T principles; anticipate powder‑bed shrinkage/expansion effects.
Nesting: maintain airflow pathways for powder removal and uniform thermal exposure.
Key Dental Applications
Orthodontics
Aligner molds, retainers, staging models, indirect bonding trays.
High‑detail edges and consistent surfaces for thermoforming predictability.
Crown and Bridge Production
Laser sintering/melting of Co‑Cr and ceramic‑related powders for frameworks and substructures.
Precision fit driven by parameter‑controlled scanning and validated finishing workflows.
Dental Implants and Surgical Guides
Patient‑specific guides improve placement accuracy and surgical efficiency.
Custom implant‑related components (non‑load bearing) with controlled tolerances and verified sterilization compatibility.
Prosthodontics
Complete and partial dentures, splints, try‑in bases, and appliance housings.
Reduced turnaround times via batch nesting and support‑free fabrication.
Maxillofacial Surgery
Patient‑specific surgical models and cutting guides.
Custom implants and anatomical references leveraging geometric freedom.
Material Requirements for Dental Applications
Low cytotoxicity: Biocompatible, safe for oral contact or proximity.
Mechanical properties: Sufficient strength, abrasion resistance, and dimensional stability.
Biocompatibility: Materials that support tissue integration where relevant.
Sterilization compatibility: Resistance to thermal, chemical, or radiation sterilization as applicable.
Biocompatibility and Safety Considerations
Biocompatible materials processed via SLS and MJF must be evaluated under ISO 10993 standards, with risk management documentation per device classification. Polymer SLS parts have shown favorable profiles for cell adhesion and proliferation in research contexts. For clinical deployment, ensure validated post‑processing (cleaning, drying, finishing), traceability, and sterilization or disinfection protocols appropriate to the device’s intended use.
Advantages of SLS/MJF for Dental Manufacturing
No support structures: Less post‑processing and material waste; easier to scale batches.
Complex geometries: Patient‑specific designs and fine lattice features for functional performance.
Production speed: MJF offers rapid cycles for aligner molds and orthodontic series; SLS scales well for medium‑sized components.
Material efficiency: Powder refresh strategies recycle unused powder, lowering cost while controlling quality.
Consistent quality: Repeatable parameters and validated workflows ensure precise fit and function.
SLS vs MJF: Comparative Insights
Process Physics
SLS: Laser scans and sinters; scan strategy and energy density control fusion and texture.
MJF: Agents tailor absorptivity; IR fuses treated areas, improving edge sharpness and speed.
Materials and Build Envelope
SLS: Broader materials, including PA11/PA12, TPU, and research composites; often taller Z capacity.
MJF: Focused materials (expanding) with strong production consistency; optimized for small to medium parts.
Accuracy, Detail, and Throughput
MJF: Excellent fine detail, crisp edges, and fast cycles for orthodontic workflows.
SLS: Tunable accuracy and surface; ideal for medium‑sized functional parts and complex nesting.
Post‑Processing and Finishing
Support‑free depowdering for both; media blasting, dyeing, or polishing based on device requirements.
Dimensional verification via GD&T, surface roughness checks (Ra), and micro‑CT or density methods.
Process Control, QA, and Compliance

Parameter Validation
SLS: Laser power, scan speed, hatch spacing, bed temperature, layer thickness.
MJF: Agent deposition density, IR lamp power, bed temperature, recoater speed, layer thickness.
Powder management: Lot traceability, refresh ratios, sieving, moisture conditioning.
Metrology and Acceptance
Orientation‑specific tensile bars to map anisotropy; dimensional checks under GD&T.
Porosity/density via micro‑CT or Archimedes; surface roughness to guide finishing.
Device History Records (DHR), calibration logs, and energy‑delivery monitoring for consistency.
Environmental and Safety
Optimize packing density and powder refresh to reduce energy and waste.
Powder handling protocols: ventilation, ESD control, personal protective equipment, and humidity management.
Decision Framework for Dental Use Cases
1. Define Clinical and Technical Constraints
Intended use, biocompatibility requirements, dimensional tolerances, and finishing targets.
2. Map Performance Requirements
Load, wear, intraoral exposure, sterilization/disinfection, and retention features.
3. Select Process
Choose MJF for small, detailed orthodontic molds and high‑throughput series.
Choose SLS for larger builds, broader materials, and complex appliance housings.
4. Validate and Pilot
Orientation studies, acceptance criteria for critical‑to‑quality features, and fit checks on sample cases.
5. Scale with QA
SPC on key dimensions, preventive maintenance, powder refresh SOPs, and traceability for FDA/ISO alignment.
XDENT LAB Perspective
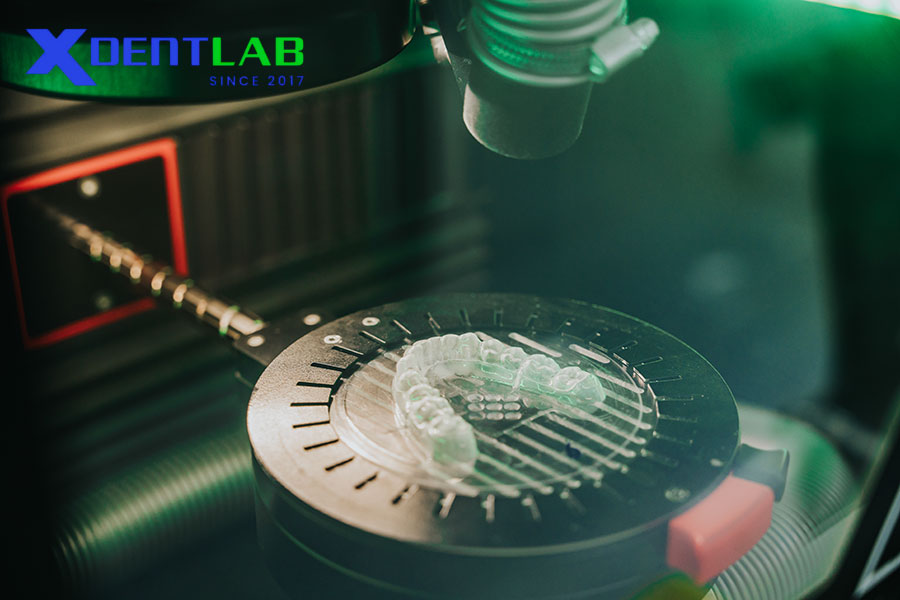
XDENT LAB delivers Lab‑to‑Lab full service from Vietnam with FDA/ISO‑aligned protocols, certified technicians, and controlled production across two factories. Our additive workflows include validated powders, documented parameters, and metrology‑driven acceptance, ensuring consistent fit, finish, and turnaround. Dental practices rely on our compliance and quality systems to scale orthodontic, prosthodontic, and surgical guide programs confidently.
XDENT LAB is an expert in Lab-to-Lab Full Service from Vietnam, with the signature services of Removable & Implant, meeting U.S. market standards – approved by FDA & ISO. Founded in 2017, XDENT LAB has grown from local root to global reach, scaling with 2 factories and over 100 employees.. Our state-of-the-art technology, certified technicians, and commitment to compliance make us the trusted choice for dental practices looking to ensure quality and consistency in their products.

Our commitments are:
100% FDA-Approved Materials.
Large-Scale Manufacturing, high volume, remake rate < 1%.
2~3 days in lab (*digital file).
Your cost savings 30%.
Uninterrupted Manufacturing 365 days a year.
Contact us today to establish a strategy to reduce operating costs.
--------❃--------
Vietnam Dental Laboratory - XDENT LAB
🏢 Factory 1: 95/6 Tran Van Kieu Street, Binh Phu Ward, Ho Chi Minh City, Vietnam
🏢 Factory 2: Kizuna 3 Industrial Park, Can Giuoc Commune, Tay Ninh Province, Vietnam
☎ Hotline: 0919 796 718 📰 Get detailed pricing
Share this post: